A Day in the Life of a Professional Caregiver
Professional caregiving in the United States is not only a vocation but a regulated profession that requires both technical skill and emotional intelligence. Every shift follows a framework of certification standards, ethical principles, and patient safety requirements. CNAs, HHAs, and PCAs together form the foundation of daily healthcare across homes and institutions.
The Structure of the U.S. Caregiving System
Caregiving in the U.S. operates under a multilayered system of federal and state oversight.
Certified Nursing Assistants (CNAs) must complete a state-approved training program, usually between 75 and 120 hours, followed by written and clinical examinations.
Home Health Aides (HHAs) are trained under federal standards established by the Centers for Medicare & Medicaid Services (CMS).
Personal Care Assistants (PCAs) may not require medical certification but often receive specialized instruction in safety, nutrition, and communication.
Continuing education is mandatory in most states to ensure caregivers stay current with infection control, fall prevention, and emergency response techniques.
The Foundations of Professional Care
Understanding the Core Roles
CNAs work in hospitals and long-term care facilities. They monitor vitals, assist with hygiene, support wound care, and document patient progress.
HHAs deliver hybrid care—combining daily living support with limited medical duties like medication reminders and mobility exercises.
PCAs provide non-medical assistance, ensuring cleanliness, safety, and emotional comfort for individuals who remain at home.
Primary Roles in U.S. Caregiving
| Role | Work Setting | Core Tasks | Focus |
|---|---|---|---|
| CNA | Hospitals, nursing homes | Vital signs, wound care, hygiene, documentation | Clinical monitoring and safety |
| HHA | Home | Meals, medication reminders, mobility assistance | Home medical support |
| PCA | Home or facility | Housekeeping, companionship, emotional care | Independence and comfort |
Daily Responsibilities and Care Priorities
ADLs and IADLs — The Core of Care
The CDC and NIH define caregiving through two fundamental task categories that sustain independence and safety.
ADLs (Activities of Daily Living)
Bathing and grooming
Feeding and dressing
Toileting and transferring
IADLs (Instrumental Activities of Daily Living)
Cooking and cleaning
Medication management
Transportation and household organization
Levels of Daily Activity Support
| Activity Type | Examples |
|---|---|
| ADLs | Bathing, dressing, eating, mobility, continence care |
| IADLs | Shopping, meal prep, cleaning, managing bills, coordinating medications |
What a Typical Day Looks Like
Morning: Active Assistance and Preparation
The morning hours are the busiest. Caregivers assist with personal hygiene, dressing, breakfast, and medication setup. These first tasks set the tone for comfort and dignity throughout the day.
Midday: Observation and Organization
Caregivers focus on nutrition, hydration, and safety checks. Documentation is continuous—intake, output, and emotional state are recorded in Electronic Health Records (EHRs).
Evening: Routine and Rest
The day ends with dinner, personal care, and emotional connection. Calm conversation and reassurance help reduce anxiety and promote healthy sleep.
Safety Protocols and Risk Prevention
Infection and Fall Prevention
Caregivers follow strict hygiene and infection-control standards. Regular handwashing, surface disinfection, and proper PPE use are critical in reducing disease transmission.
Medication and Emergency Safety
Medication schedules must be verified daily, and any side effects promptly reported. Emergency plans—fire, fall, or sudden illness—are practiced and logged as part of safety drills.
According to the CDC, caregivers often act as the first line of defense by recognizing early signs of decline—such as fatigue, dizziness, or appetite loss—helping prevent acute hospitalizations.
Technology in Modern Home Care
Digital tools have transformed the caregiving landscape.
Electronic Health Records (EHRs) streamline documentation and physician updates.
Remote patient monitoring enables real-time vitals tracking for at-risk clients.
Telehealth platforms such as Doctor2me connect home caregivers with physicians for timely evaluation and medication adjustments.
Technology doesn’t replace human care—it strengthens the safety net by linking every participant in the care continuum.
Specialized Training and Emotional Intelligence
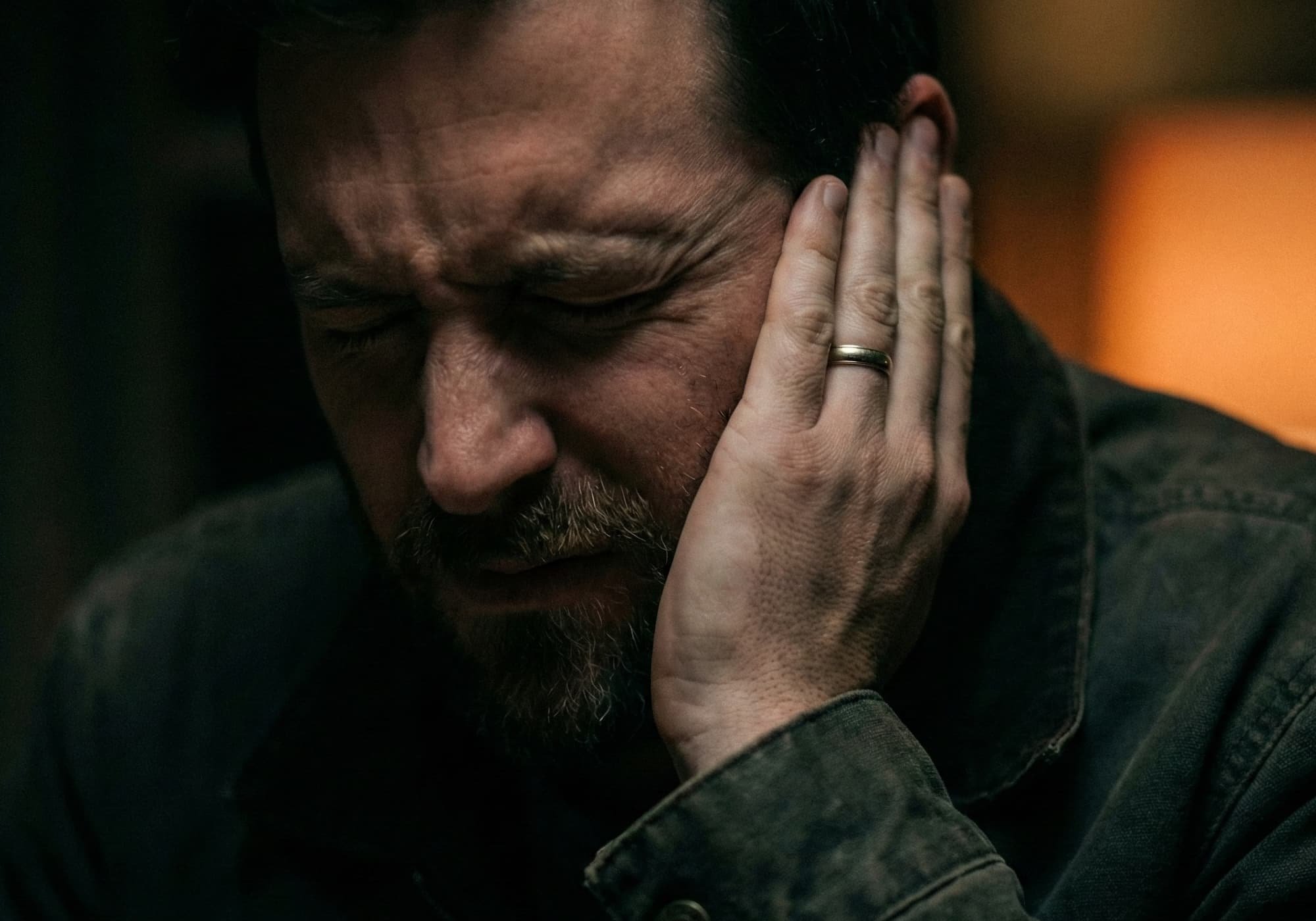
Empathy as a Core Competency
Caregivers are trained not only in physical assistance but in empathy and emotional regulation. Gentle tone, patience, and nonverbal reassurance are often more therapeutic than medication.
Working with Dementia and Behavioral Changes
Predictable routines, reduced sensory stimuli, and one-step guidance help clients with dementia feel grounded. Caregivers learn to respond calmly to resistance or confusion, avoiding escalation and fear.
Supporting Mental Health
Many caregivers now receive mental health training to recognize signs of depression, anxiety, or social withdrawal in their clients. Compassionate listening and coordination with mental health professionals are key parts of daily care.
Collaborative Network of Care
Hospice and End-of-Life Care
Hospice professionals such as Liem Hospice focus on comfort, symptom control, and emotional connection. Collaboration between caregivers and hospice teams ensures dignity and peace for patients and families alike.
Geriatric Coordination and Preventive Medicine
Working alongside geriatric specialists such as Dr. Rebecca Cook, M.D., caregivers help bridge clinical recommendations with daily routines. This integrated model supports chronic condition management and preventive care at home.
Equipment and Accessibility
Providers like Medlife Medical Supply deliver essential medical devices—hospital beds, oxygen systems, and lifts—that make complex home care safe and efficient. Proper equipment reduces caregiver strain and prevents patient injuries.
Transitional Support Services
Organizations such as Senior Home Transitional Services assist families with relocation, home adjustments, or financial planning when moving between levels of care. These services ease stress and keep continuity during transitions.
Documentation, Ethics, and Professional Standards
Caregivers are required to document every intervention accurately—vitals, meal intake, behavior changes, and incidents. This transparency supports accountability and continuity.
Confidentiality under HIPAA is strictly enforced: personal information is shared only with authorized medical professionals. Ethical caregiving also means respecting boundaries, promoting autonomy, and reporting any potential neglect or abuse immediately.
Supporting the Caregiver
Preventing Burnout and Fatigue
Physical exhaustion and emotional fatigue are common in the caregiving profession. Strategies include scheduled breaks, group support, and proper sleep routines. According to the CDC, self-care directly affects caregiver retention and patient outcomes.
Accessing Respite and Community Resources
Respite Care programs provide temporary relief for both family and professional caregivers. Transitional services help prevent burnout during prolonged care. Maintaining a balanced schedule is critical for sustainable work.
The Future of Caregiving in the United States
The caregiving field is evolving rapidly. As the population ages, demand for qualified professionals is rising. The future depends on integrating human empathy with technological precision—combining mobile diagnostics, telehealth, and strong professional education.
By promoting collaboration between doctors, caregivers, and support providers, the U.S. can build a sustainable model of compassionate care—one that values both patient dignity and caregiver well-being.
Professional caregiving is not an auxiliary service—it’s the foundation of community health. The cooperation of skilled caregivers, geriatric physicians, hospice teams, equipment suppliers, and transitional coordinators creates a holistic system that allows aging adults to live safely, independently, and with dignity in the place they call home.
FAQ
1. What are the steps to obtain and maintain certification for each caregiving role in my state?
Certification depends on state regulation, but the process generally follows a consistent path across the U.S.:
To obtain certification:
CNAs: complete a 75–120-hour state-approved program and pass both written and clinical exams.
HHAs: meet federal CMS standards and complete 75 hours of hands-on training.
PCAs: complete employer-based or state-specific non-medical care instruction.
To maintain certification:
Renew the license on schedule (usually every 1–2 years).
Complete required continuing education hours.
Stay updated on infection control, safety, and documentation standards.
2. Can you provide real-life examples or scenarios of handling challenging patient behaviors?
Experienced caregivers face behavioral challenges daily, often requiring empathy and creativity.
A client with dementia might resist bathing out of confusion or fear. The caregiver uses calm tone, soft lighting, and clear, simple options — “Would you like warm or cool water?” — to restore trust and comfort.
In another case, a patient in chronic pain becomes irritated during mobility exercises. The caregiver pauses the routine, acknowledges the discomfort, and resumes at a slower pace. These adjustments preserve the client’s dignity and maintain cooperation.
3. What specific digital tools or EHR platforms are most commonly used in home care settings?
Technology now drives most home care coordination. The most common tools include:
MatrixCare, AlayaCare, and ClearCare: for digital charting, vitals tracking, and shift documentation.
Doctor2me: for secure telehealth communication between caregivers and physicians.
Mobile caregiver apps: for scheduling, GPS check-ins, and secure messaging.
These platforms reduce paperwork, prevent documentation errors, and help maintain real-time coordination between the entire care team.
4. How can new caregivers access support groups or respite care resources in their local area?
Support is essential to prevent emotional burnout. New caregivers can start locally:
Community Area Agencies on Aging (AAA) provide directories for respite care and caregiver programs. National groups such as the Family Caregiver Alliance and Alzheimer’s Association offer online and in-person peer support.
Hospitals and home health agencies often hold small local meetings for caregivers to share challenges and strategies. Many caregivers also join private online communities for daily advice, resource sharing, and emotional connection.
5. What are the typical career advancement paths for CNAs, HHAs, and PCAs?
Caregiving offers structured and meaningful career growth opportunities:
PCA → CNA: gaining clinical certification opens new job settings and responsibilities.
CNA → LPN or RN: pursuing nursing school leads to broader clinical authority and higher responsibility.
Specialization: experienced caregivers may advance into hospice coordination, wound care, or dementia support.
Leadership: others move into supervisory, training, or case-management roles, mentoring new caregivers.
Each step builds on practical experience and deepens the professional’s impact on patient outcomes.
You May Also Like