Discussing Sensitive Topics With Your Doctor
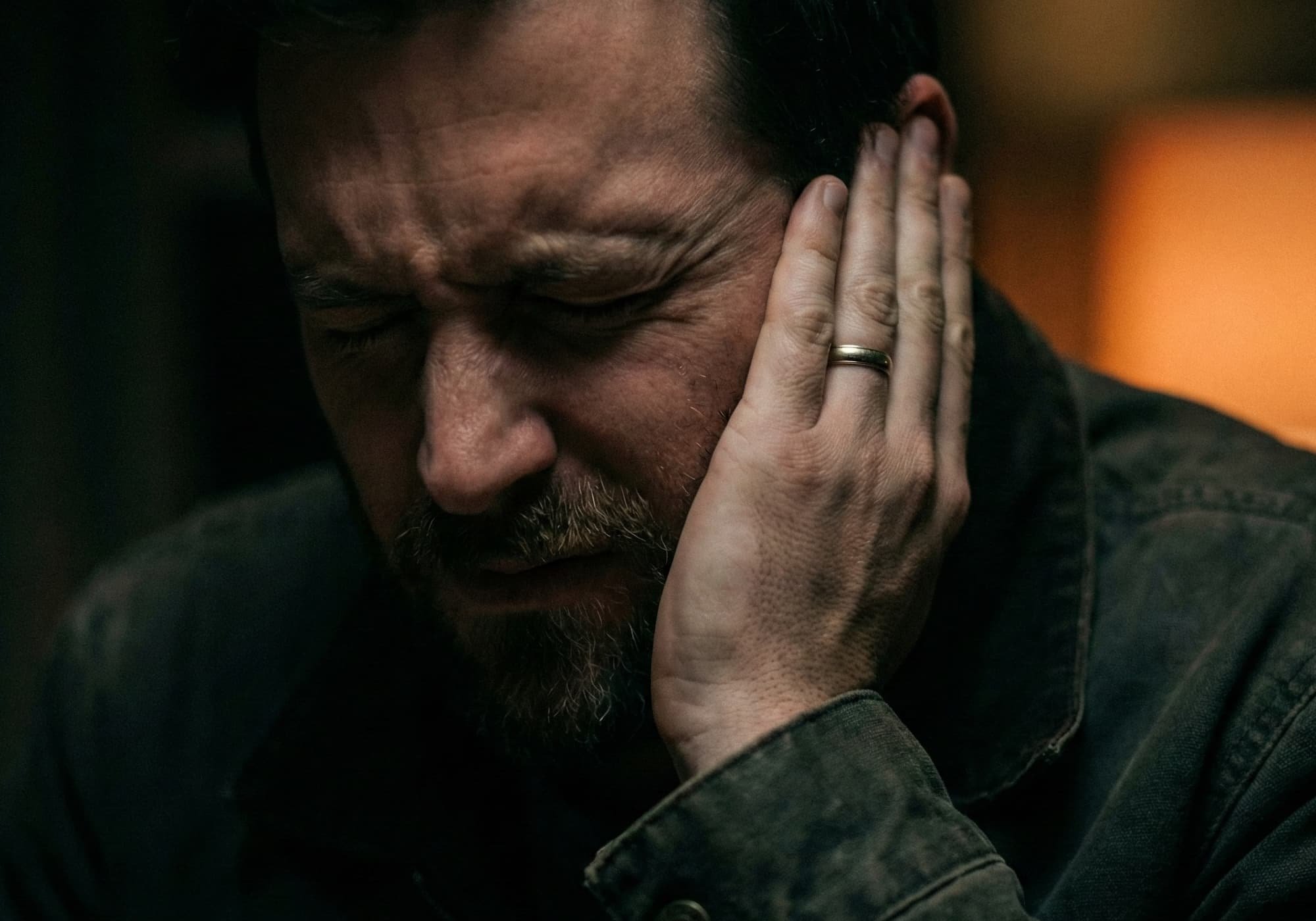
Feeling embarrassed or unsure can delay care and hide crucial facts. Discussing sensitive topics with your doctor gives clinicians the full picture, reduces diagnostic delays, and helps prevent dangerous medication conflicts.
Why Honest Conversations Protect Health
Specific details connect symptoms, risks, and timelines. When a person downplays alcohol use, sexual health concerns, mental-health history, or non-prescribed substances, the plan can miss. Honest disclosure lets the doctor choose safer tests and treatments, set realistic goals, and reduce stress during visits.
Small facts matter. A weekend supplement, an over-the-counter sleep aid, a past panic attack, or a new partner can change what is safe to prescribe and which screening is needed. Discussing sensitive topics with your doctor turns these details into protection.
Privacy And Psychological Safety
Many stay silent from fear of judgment or disclosure. In the United States, federal privacy rules (HIPAA) require clinics to safeguard personal health information. Clinicians also follow ethical standards that prioritize confidentiality and respectful care.
A good visit feels safe: the room is calm, the doctor listens, and language stays neutral. If a topic is hard to start, preface it with: “This is uncomfortable to say, but it affects my care.” Most clinicians welcome candor and adjust their pace accordingly.
How To Start A Delicate Conversation
Opening lines reduce anxiety and set a practical tone. Use one approach and then move to specifics.
Normalize The Topic
Say, “People often struggle to bring this up, but I need to talk about…” This signals that empathy—not judgment—is expected.
Lead With Safety
Explain the reason: “I want to avoid bad reactions with my medicines,” or “This could change which tests I need.” Safety is a shared goal.
Name The Concern Clearly
Avoid vague phrases like “something is off.” Describe what hurts, when it began, what worsens it, and what helped. Specifics beat euphemisms.
Practical Prep Before The Visit
Preparation turns nerves into facts and keeps the visit focused.
Write the top three concerns. Put the most delicate first.
Draft a symptom timeline: onset, frequency, severity (0–10), triggers, relief.
Bring a complete med list: doses, vitamins, supplements, herbals, occasional sleep aids, and recreational substances.
These steps reduce guesswork and prevent unsafe interactions.
Straight Talk About Common “Hard” Topics
Delicate does not mean rare. Many people face similar issues and feel the same hesitation. Be direct and tie each point to care decisions.
Substance Use (Alcohol, Cannabis, Stimulants, Opioids)
Be exact about what, how much, and how often. If cutting back or worried about dependence, say so. Doctors adjust medications, monitor organ risks, and plan safer tapers when they know the details.
Sexual Health And Intimate Safety
Discuss partners, protection, pregnancy intentions, genital symptoms, pain with intercourse, or exposure concerns. Precision guides STI testing, vaccinations, contraception, and referrals. If there is coercion or violence, sharing that can unlock medical and community support.
Mental Health And Medications
List current and past diagnoses, therapy, hospitalizations, and all psych meds—including recent stops. Many drugs interact with antidepressants, mood stabilizers, or anxiety treatments. Openness avoids serious reactions and helps balance physical and mental-health goals.
Weight, Eating Patterns, And Body Image
If weight talks feel shaming, say so. Ask to anchor the plan in function, energy, sleep, blood pressure, and labs—not only the scale. Boundaries and practical help can coexist.
Scripts You Can Borrow
Short sentences work best. Adapt as needed.
“This feels awkward, but it affects my treatment: I use [substance] about [amount/frequency]. I want to prevent medication conflicts.”
“I’ve had pain during sex for three months. It’s sharp, internal, worse with penetration. I’d like an exam and guidance.”
“I stopped my antidepressant two weeks ago due to side effects. Since then I sleep poorly and feel on edge.”
“Weight talks are tough for me. Can we focus today on stamina, blood pressure, and knee pain while planning healthy habits?”
Use one line to open the door, then add details.
A Simple Framework For Sensitive Visits
| What To Bring Or Say | Why It Helps |
|---|---|
| Top-3 concerns, with the most delicate first | Guarantees the key topic gets time and focus |
| Symptom timeline with triggers and severity | Speeds diagnosis and avoids guesswork |
| Full list of meds, vitamins, supplements, substances | Prevents dangerous drug interactions |
| One clear opening line (safety or normalization) | Sets a respectful, non-judgmental tone |
Your Role As An Equal Partner
Patients can shape the visit. If a topic needs more time, ask the front desk when scheduling. During the appointment, request plain language: “Could you explain that in simple terms and outline my options?” If you feel rushed, pause: “This point affects my safety; can we stay with it for a minute?” A trusted support person can help you remember details and advocate calmly.
If a clinician ignores boundaries or uses shaming language, it is reasonable to seek another provider who practices respectful, person-centered care. Competent medicine and a supportive environment should come together.
House-Call Or Virtual Settings For Sensitive Discussions
Some conversations feel easier at home. When appropriate, a house-call or private video visit can reduce stress, allow a supporter to join, and make it simple to show medications and devices on the spot. The same rules apply: prepare your top three concerns, speak plainly, and lead with safety. For older adults or people with mobility limits, in-home care also reduces exposure to crowded clinics.
Quick Lists You Can Use Today
Three Things To Say Up Front
“I’m sharing this to keep my treatment safe.”
“Here are my top three concerns—can we start with the first one?”
“I use [specific substance/med/supplement] at [dose/frequency].”
Three Things To Bring
Up-to-date med/supplement list with doses
Written symptom timeline
A support person (in-person or by phone), if helpful
These habits lower anxiety and improve care quality immediately.
Gentle Next Steps
If a delicate concern is on your mind, write one sentence that names it and one question you want answered. Schedule a visit and use your opening line in the first minute. Keep your note with your med list so you don’t need to improvise under stress. Discussing sensitive topics with your doctor is a skill; it gets easier with practice.
Building this habit of openness becomes easier with the right setting. For many, that means a calm, private visit at home. Doctor2me house-call physicians provide exactly that—confidential in-room or virtual consultations where sensitive concerns can be raised without pressure. By combining medical expertise with privacy, they make it simpler to share delicate details and receive safe, tailored guidance.
FAQ
Why is discussing sensitive topics with your doctor important?
Honest disclosure ensures safe treatment, prevents drug interactions, and helps doctors choose the right tests and care plans.What if I feel too embarrassed to talk about certain issues?
Start with a simple line like, “This is hard to say, but it affects my care.” Doctors are trained to respond respectfully.How do I prepare before bringing up delicate concerns?
Write down your top three concerns, make a symptom timeline, and prepare a complete list of medications and supplements.Can I bring someone with me for support?
Yes. Having a trusted friend or family member present can reduce anxiety and help you remember key details.Is a house-call or virtual visit a good option for sensitive conversations?
For many, yes. Home or virtual visits provide privacy, reduce stress, and make it easier to speak openly.
You May Also Like